Customary paradigm in anesthetic management of carotid endarterectomy patients shifts after pandemic: experiences of an advanced practice centre

| Available Online: | January, 2025 |
| Page: | 3–7 |
Author for correspondence:
Prof. Elvin Kesimci, MD, PhD
Baskent University Medical Faculty, Department of Anesthesiology,
Fevzi Çakmak Cd 10. Sok. No:45, 06490 Bahçelievler/Ankara, Turkey
Tel: +90 312203 68 68 – 4855
E-mail: dr.ahmed.elshiekh1@gmail.com
ISSN 2732-7175 / 2025 Hellenic Society of Vascular and Endovascular Surgery
Published by Rotonda Publications
All rights reserved. https://www.heljves.com
2 Department of Cardiovascular Surgery, Başkent University Faculty of Medicine, Ankara, Turkey
Abstract
Full Text
References
Images
Abstract
Purpose: During the COVID-19 pandemic, aerosol-generating procedures posed significant infection risks to operating room (OR) staff. This study evaluated the shift from regional anesthesia (RA; cervical plexus block) to general anesthesia (GA) with rapid sequence intubation (RSI) for carotid endarterectomy (CEA) patients, aiming to minimize viral transmission while maintaining patient safety.
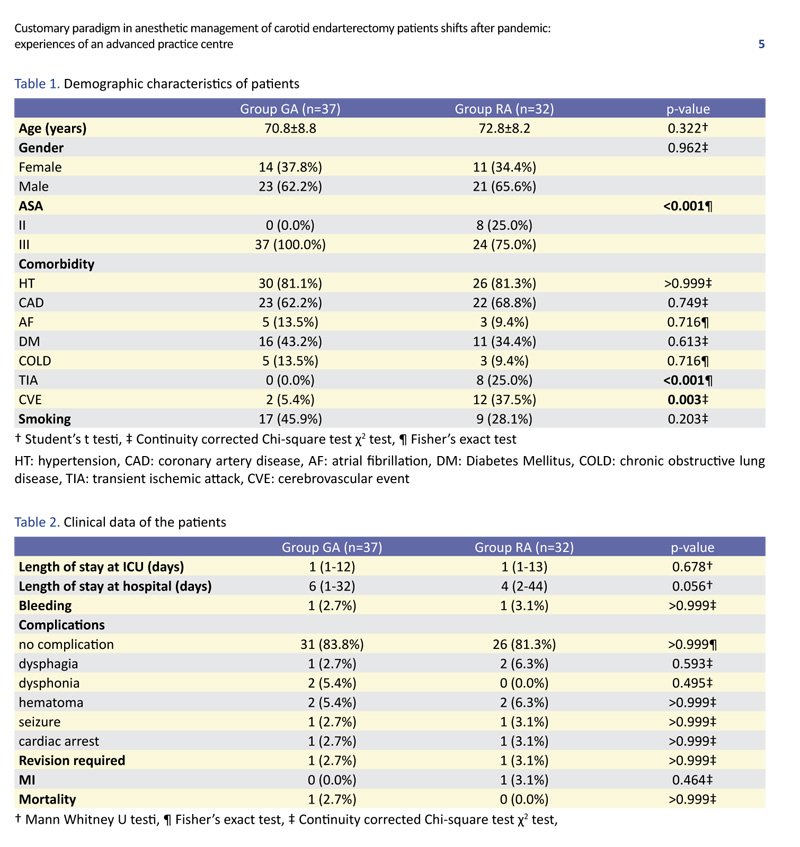
Materials and Methods: A retrospective analysis was conducted on 69 CEA patients treated between May 2019 and May 2021. Among them, 32 received RA (pre-pandemic) and 37 received GA (during the pandemic). Collected data included demographics, comorbidities, anesthesia type, ICU and hospital stay duration, and complications. RA was performed using an ultrasound-guided cervical plexus block, while GA utilized RSI with videolaryngoscopy and strict aerosol-control measures. Statistical analysis compared outcomes between the two groups.
Results: There were no significant differences in age, gender, or ICU/hospital stay between the two groups. GA patients had higher ASA scores (p<0.001), while RA patients experienced more cerebrovascular events. Complications related to RA—such as dysphagia, coughing, and respiratory distress—increased aerosolization risks, prompting the transition to GA. Importantly, no COVID-19 transmission was recorded among OR staff during GA procedures.
Conclusion: Although RA has been the traditional approach for CEA, GA with RSI proved safer for OR personnel during the pandemic without compromising patient outcomes. This paradigm shift underscores the need to adapt anesthetic strategies during public health crises, prioritizing staff protection during aerosol-generating procedures while maintaining optimal patient care.
Keywords: Carotid endarterectomy, COVID-19, general anesthesia, regional anesthesia, aerosol-generating procedures, rapid sequence intubation.
Full Text
INTRODUCTION
Anesthesiologists and operating room (OR) staff are exposed to infectious droplets and aerosols during airway management. In ORs, anesthesiologists must take strict precautions to reduce aerosol-generating procedures in order to prevent the spread of infections to other patients and healthcare workers. General anesthesia (GA) and rapid sequence induction (RSI) are both recommended to reduce airborne and droplet transmission through the patient’s mouth and nose during the COVID-19 outbreak.
Carotid endarterectomy (CEA) has been accepted as the “gold standard” treatment option for symptomatic patients since 1970. However, these patients often have multiple comorbidities and are prone to intraoperative hemodynamic deteriorations. Therefore, a personalized anesthetic management approach is required. The choice between GA and regional anesthesia (RA) for CEA has been widely debated due to the distinct advantages and disadvantages of each technique. Although both methods share similar goals, there is no consensus on the preferred anesthetic technique, as the decision usually depends on the institution’s experience and comfort level.
At our center, RA has traditionally been the first-choice anesthetic management technique for CEA patients. However, complications related to cervical plexus block—such as anxiety, paroxysmal coughing, shortness of breath, airway obstruction, dysphagia, and the potential need for emergent orotracheal intubation—necessitated a change in our customized anesthetic approach during the COVID-19 outbreak. Although endotracheal intubation is generally considered a high-risk procedure, even under elective conditions, we chose GA over RA for CEA patients at our center during this period.
Our aim was to guide cardiovascular teams in managing CEA patients in a way that protects both patients and medical staff, contributing to public health efforts to mitigate infection spread during the pandemic.
MATERIALS AND METHODS
After obtaining approval from the Clinical Research Ethics Committee of Başkent University Faculty of Medicine (KA22/396), 69 patients who underwent CEA at Başkent University Ankara Hospital between May 2019 and May 2021 were retrospectively analyzed. Due to the onset of the COVID-19 outbreak, 37 patients (February 2020–May 2021) received GA, while 32 patients (May 2019–January 2020) underwent cervical plexus block. Patient files were reviewed to collect data on demographics (age, gender, BMI), comorbidities, type of anesthesia and operation, ICU and hospital stay durations, and any complications. Patients who underwent simultaneous CEA with coronary artery bypass or valve surgery were excluded.
Anesthesia Management
No premedication was given. All patients had intravenous (IV) access established, and standard monitoring included ECG, pulse oximetry, and invasive blood pressure measurement via the contralateral radial artery.
In the RA group, oxygen (2 L/min) was administered nasally. The cervical plexus block was performed by a senior anesthesiologist with the patient in a supine position and the head slightly turned away. The sternocleidomastoid muscle, cricoid cartilage, and mastoid process were identified. Under ultrasound guidance, a needle was advanced into the carotid sheath and then to the anterior border of the sternocleidomastoid muscle at the level of C6. A total of 20 mL local anesthetic (5 mL 0.5% bupivacaine and 5 mL 2% prilocaine) was administered perivascularly in two doses. Surgery began once adequate sensory blockade was confirmed. If analgesia was insufficient, local infiltration with 1% lidocaine was performed. Patients were monitored for neurological and motor responses during surgery.
After the COVID-19 outbreak, GA became the preferred technique. Cerebral oximetry (NIRS) was used before and during anesthesia induction. Induction included IV lidocaine (1 mg/kg) to suppress hemodynamic responses, fentanyl (2 μg/kg), and rocuronium bromide (0.6 mg/kg) for muscle relaxation. Orotracheal intubation was performed, and mechanical ventilation was applied with 4–6 mL/kg tidal volume and respiratory rates of 12–16/min to maintain end-tidal CO₂ between 30–35 mmHg. Anesthesia was maintained with sevoflurane (0.8–1.1%) or desflurane (5–6%) in an oxygen/air mixture (FiO₂ = 50%). At the end of surgery, the anesthetic agent was discontinued, sugammadex was administered, and extubation was performed after confirming neurological function.
During surgery, hypovolemia or hypotension was treated with IV crystalloids and, if necessary, norepinephrine boluses or infusions. Hypertension was managed with nitroglycerine boluses. All patients were transferred to the ICU postoperatively for monitoring.
Statistical Analysis
Data analysis was conducted using IBM SPSS Statistics v25. Normality was assessed using the Kolmogorov-Smirnov test. Categorical variables were expressed as numbers and percentages, and quantitative data as mean ± SD or median (min–max). Student’s t-test or Mann-Whitney U test was applied as appropriate. Categorical variables were analyzed using Chi-square or Fisher’s exact test. A p-value <0.05 was considered statistically significant.
RESULTS
Between May 2019 and May 2021, 69 patients (25 females, 44 males) underwent CEA for carotid artery stenosis. Of these, 37 patients (14 females, 23 males) received GA with orotracheal intubation (Group GA), and 32 patients received RA (Group RA). There were no significant differences in mean age or gender distribution between the groups (p=0.322 and p=0.962, respectively).
Group GA had significantly higher ASA scores (p<0.001), but comorbidities were comparable between groups. A history of cerebrovascular events (CVE) and transient ischemic attacks (TIA) was more common in Group RA. ICU and hospital stay durations were similar between groups.
DISCUSSION
The COVID-19 pandemic led to substantial changes in anesthetic practices worldwide. At Başkent University Hospital, our cardiovascular surgery and anesthesiology teams had previously performed 483 CEA operations under cervical plexus block between 2003 and early 2020. However, due to the pandemic, our anesthetic approach shifted to GA.
While deep cervical plexus block remains an effective anesthetic method for assessing neurological and motor function, it carries the risk of complications such as difficulty swallowing, paroxysmal coughing, shortness of breath, airway obstruction, and the need for emergency intubation—all of which increase aerosol generation and environmental contamination. Considering the infection risks during the pandemic, we introduced modifications to our perioperative management, despite our extensive experience with RA.
Previous studies have reported successful CEA operations under cervical plexus block, with Stoneham and colleagues demonstrating its feasibility using deep or superficial blocks combined with local infiltration. However, the incidence of phrenic nerve paralysis was not well defined. Although few complications were reported, most studies focused on surgical outcomes rather than intraoperative respiratory or neurological deterioration—issues of primary concern for anesthesiologists.
Deep cervical blocks, in particular, are associated with higher rates of complications compared to superficial or intermediate ones due to the complex vascular and neural anatomy of the neck. These blocks can affect the recurrent laryngeal, vagus, hypoglossal, and phrenic nerves, potentially impairing respiratory function. Opperer et al. highlighted the impact of block depth on hemidiaphragmatic movement due to phrenic nerve palsy, noting measurable but clinically insignificant respiratory changes.
In our experience, transient respiratory issues such as dyspnea, coughing, desaturation, and dysphagia were common with RA, and during the pandemic, these became high-risk aerosol-generating situations. Moreover, because RA was not initially perceived as an aerosol-generating technique, staff might have used personal protective equipment less rigorously. For this reason, we transitioned to GA with RSI, using videolaryngoscopy and protective barriers to minimize exposure.
In the broader literature, RA continued to be preferred for non-airway-related surgeries—such as orthopedic, urological, and obstetric procedures—during the pandemic. However, given the proximity of the surgical field to the airway in CEA, GA proved safer for staff in our setting. Topcu et al. similarly reported a higher rate of RA use during the pandemic, though hospital contexts varied.
Our institution, being a tertiary private university hospital specializing in cardiac and transplant surgery, handled older and higher-risk patients, often referred from state hospitals. The reduction in TIA and stroke cases during the pandemic may also reflect lower diagnosis rates overall.
In summary, the COVID-19 pandemic significantly influenced our anesthetic practice for CEA. Transitioning from RA to GA with RSI protected healthcare staff without compromising patient outcomes. Strict adherence to infection control protocols ensured optimal safety and successful results.
References
Images