Spontaneous aneurysm of the right external jugular vein

| Available Online: | January, 2025 |
| Page: | 25–27 |
Author for correspondence:
Simlawo Kpatékana
University Hospital Center of Sylvanus Olympio, Togo
Tel: (00228) 90367573
E-mail: richardsim82@yahoo.fr
ISSN 2732-7175 / 2025 Hellenic Society of Vascular and Endovascular Surgery
Published by Rotonda Publications
All rights reserved. https://www.heljves.com
2University Hospital Center of Sylvanus Olympio, Togo
Abstract
Full Text
References
Images
Abstract
External jugular vein aneurysms (EJVAs) are rare vascular anomalies, typically presenting as asymptomatic, soft, and compressible neck masses that become more prominent with increased intrathoracic pressure.
This report details the case of a 69-year-old woman with a progressively enlarging right-sided cervical mass, accentuated by laughing. Imaging via Doppler ultrasound confirmed a pseudoaneurysm of the right external jugular vein, characterized by a parietal breach and a compressible venous sac. Surgical resection with end-to-end anastomosis was successfully performed, with an uneventful postoperative course.
EJVAs may be congenital or acquired, with risk factors including venous insufficiency, aging, and prior trauma, although many cases remain idiopathic. Diagnosis relies on clinical examination and imaging, with Doppler ultrasound as the primary tool.
Treatment is typically surgical, mainly for aesthetic reasons, though endovascular options exist. This case underscores the importance of considering EJVA in the differential diagnosis of lateral neck masses and highlights the role of imaging in guiding management.
Full Text
INTRODUCTION
Venous aneurysms are relatively rare lesions that have been reported throughout the venous system. They occur most often in the lower limbs, followed by the face, neck, abdomen, and thorax. Cervical aneurysms are even rarer and generally involve the internal jugular vein. External jugular vein aneurysms (EJVAs) are rare and often pose an aesthetic concern. We report a case of spontaneous aneurysm of the external jugular vein and describe the circumstances of its discovery and therapeutic management in a 69-year-old female patient.
OBSERVATION
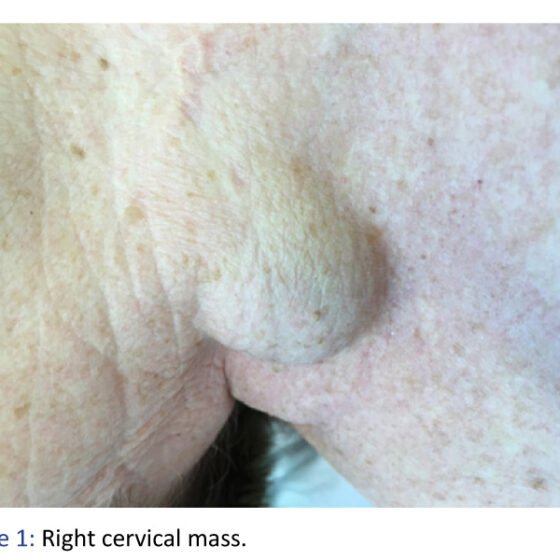
A 69-year-old female patient presented with a visible mass on the right side of the neck, which had gradually increased in size and became more prominent when she laughed.
Her medical history included chronic venous insufficiency. There was no history of catheterization of the internal or external jugular veins, and no prior cervical trauma. She had been followed for varicose veins and had undergone sclerotherapy.
Physical examination of the cervical region revealed a mass at the base of the neck, located on the right side and slightly lateral to the neck vessels, measuring approximately 2 cm in diameter. The mass expanded with respiratory movements. It was soft, compressible, non-fluctuant, non-pulsatile, and without a thrill. The overlying skin was neither erythematous nor inflamed. No other masses or lymphadenopathy were detected elsewhere in the neck. Auscultation revealed no murmur.
Ultrasonography with color Doppler of the neck vessels revealed the following findings:
-
Right side: The common carotid artery, its bifurcation, and both the internal and external carotid arteries were patent and without abnormality. The right thyroid lobe appeared normal. The right subclavian and vertebral arteries in segments V0 and V1 were also normal. The internal jugular vein was unremarkable. A venous mass, visible externally, was supplied by the external jugular vein. A clearly visible breach in the wall of the external jugular vein allowed communication with a venous pocket located laterally in the neck. Color Doppler imaging showed filling of the venous sac with each respiratory movement and during intrathoracic pressure exertion. The venous pocket measured 1.5 cm in thickness and 3 cm in diameter, was fully compressible, and showed no signs of thrombosis. These findings were consistent with a true false aneurysm of the right external jugular vein.
-
Left side: The supra-aortic trunks and jugular veins were normal.
The patient underwent surgical resection of the aneurysm with end-to-end anastomosis under general anesthesia. Postoperative recovery was uneventful, and the patient was discharged on postoperative day 4.
DISCUSSION
Venous aneurysms are rare compared to arterial aneurysms. Over a span of 21 years, only five cases of venous aneurysms were reported, of which only two were external jugular vein aneurysms. The most common site for cervical venous aneurysms is the internal jugular vein.
Several differential diagnoses have been proposed for a lateral cervical mass, including upper mediastinal tumors and cysts, external laryngeal diverticulum, and venous aneurysms. Venous aneurysms can be either congenital or acquired. Among the acquired forms, risk factors include recent trauma, aging, cardiovascular disease, inflammation, venous insufficiency, and arteriovenous fistulas. In some cases, no clear etiology is identified.
In this case, there was no history of recent trauma or catheterization of the cervical veins. The patient was 69 years old and under follow-up for chronic venous insufficiency. Notably, cases of cervical venous aneurysms involving the internal jugular vein have even been reported in infants as young as 3 and 6 months old.
EJVA typically presents as a unilateral, asymptomatic, oval mass that is non-pulsatile and silent on auscultation. Its most distinctive feature is the increase in size during laughter, shouting, or Valsalva maneuvers. However, clinical examination alone often cannot distinguish it from aneurysms of the internal jugular vein. Diagnostic approaches remain debated. While Doppler ultrasound is often sufficient for diagnosis, computed tomography offers superior spatial and temporal resolution and is better suited for detecting vascular anomalies.
Surgical management of venous aneurysms of the neck and face is not as systematic as for other venous aneurysms, which are typically operated on to prevent complications such as pulmonary embolism, hemorrhagic rupture, or compression. In the case of cervical and facial venous aneurysms, surgery is usually performed for cosmetic reasons.
Regarding therapeutic options, two approaches are available: open surgery, which is the most commonly performed, and endovascular surgery. Open surgical techniques include ligation, tangential venorrhaphy with or without aneurysm resection, and venous bypass.
Endovascular surgery offers aesthetic advantages, especially for aneurysms in the cervical or facial regions. It can be performed on an outpatient basis and under local anesthesia. The procedure involves catheterizing the aneurysm via a femoral approach and embolizing it.
CONCLUSION
External jugular vein aneurysms are extremely rare and typically present as cosmetic concerns. They may be congenital or acquired, with no identifiable cause in some cases. Surgical treatment, most often via open techniques, is the standard approach, with endovascular procedures used in select cases.
References
-
J.-L. Gillet: Anévrismes veineux. Journal des Maladies Vasculaires. 2015;40:73–74.
-
David Ryan Chapman, Raymond Elliot Ho, Antonio Gangemi: A case report of a rare, spontaneous external jugular vein aneurysm. International Journal of Surgery Case Reports. 2018;52:8–10.
-
Sessa C, Perrin M, Nicolini P: Anévrismes veineux. EMC-Chirurgie. 2005;2:317–331.
-
Roshan Kumar Verma, Darwin Kaushal, Naresh K. Panda: External Jugular Vein Aneurysm with Thrombus Presenting as Painful Neck Mass. A Case Report. Oman Medical Journal. 2013;28:278–280.
-
Senthil Kumar Aiyappan, Upasana Ranga, Saveetha Veeraiyan: Aneurysm of External Jugular Vein Mimicking Hemangioma of Neck. Indian Journal of Surgery. 2013;75:493–495.
-
Drakonaki E.E., Symvoulakis E.K., Fachouridi A., Kounalakis D., Tsafantakis: External jugular vein aneurysm presenting as a cervical mass. International Journal of Otolaryngology. 2011;485293.
-
Joe B. Baker, Christopher R. Ingraham, Gabriel C. Fine, Ramesh S. Iyer, Eric J. Monroe: Pediatric jugular vein aneurysm (phlebectasia): report of two cases and review of the literature. Radiology Case Reports. 2017;12:391–395.
-
Rajadurai A., Abdul Aziz A., Mat Daud N.A., Abdul Wahab A.F., Muda A.S.: Embolisation of external jugular vein aneurysm: a case report. Malaysian Journal of Medical Sciences. 2017;24:107–112.
-
Andreev A., Petkov D., Kavrakov T., Penkov P.: Jugular venous aneurysms: when and how to operate. International Angiology. 1998;17:272–275.
-
Bosshardt T.L., Honig M.P.: Congenital internal jugular venous aneurysm: diagnosis and treatment. Military Medicine. 1996;161:246–247.
-
Calligaro K.D., Ahmad S., Dandora R., Dougherty M.J., Savarese R.P., Doerr K.J., et al.: Venous aneurysms: surgical indications and review of the literature. Surgery. 1995;117:1–6.