Biopsychosocial Assessment and Intervention on Vascular Diseases of Lower Extremities

| Available Online: | April, 2023 |
| Page: | 135-138 |
Author for correspondence:
Eliza (Eleni- Zacharoula) Georgiou
Department of Psychiatry, Patras University General Hospital, University of Patras, Rio 26504, Patras, Greece
E-mail: elizageo8@gmail.com
doi: 10.59037/hjves.v4i4.5
ISSN 2732-7175 / 2022 Hellenic Society of Vascular and Endovascular Surgery Published by Rotonda Publications
All rights reserved. https://www.heljves.com
Eliza (Eleni- Zacharoula) Georgiou1 , Savvina Prapiadou2 , Anastasia Xynogala2 , Andreas Tsimpoukis3 , Panagiotis Alexopoulos1,2,4,5,6, Konstantinos Moulakakis3
1 Department of Psychiatry, Patras University General Hospital, University of Patras, Greece 2 Medical School, University of Patras, Greece 3 Department of Vascular Surgery, Patras University General Hospital, University of Patras, Greece 4 Global Brain Health Institute, Medical School, Trinity College Dublin, The University of Dublin, Dublin, Republic of Ireland 5 Department of Psychiatry and Psychotherapy, Klinikum rechts der Isar, Faculty of Medicine, Technical University of Munich, Munich, Germany 6 Patras Dementia Day Care Centre, Patras, Greece
Abstract
Full Text
References
Abstract
Introduction: Peripheral arterial disease (PAD), which involves one or more vessels of the lower extremities, is common in older adults due to complex genetic and environmental interactions that result in reduced peripheral perfusion. Despite being in many cases asymptomatic, early PAD is associated with reduced survival rate due to its undeniable association with atherosclerosis in other arterial areas, such as the coronary, carotid and cerebral circulations. As population worldwide grows and ages and modern lifestyle leading to obesity and Diabetes Mellitus becomes more popular the number of older adults affected by lower extremity lesions due to PAD increase. While the biological consequences of these diseases have been well-studied, the highly prevalent neuropsychiatric aftermath of vascular diseases has yet to be thoroughly investigated.
Methods: The conduction of this review was made possible with the use of the databases PubMed and Google Scholar and articles were included up until November 2022. Only peer-reviewed journal articles were eligible. Key words used include combinations of the terms “PAD”, “Psychiatric diseases”, “vascular diseases”, “diabetes”, “anxiety”, “depression”, “psychological status”, “cognition” and “amputation”.
Results: The few studies that have assessed the psychological status of patients with vascular diseases suggest that psychiatric comorbidities are common in this patient group. Further larger scale studies are needed to elucidate the exact mechanism of this phenomenon as well as the optimal diagnostic methods, treatment plan and intervention timeline for these patients.
Conclusion: In the present review light is shed on mental illness symptoms in PAD and their importance for disease management and course as well as the quality of life of patients.
Full Text
INTRODUCTION
Peripheral arterial disease (PAD) is a serious health care issue for older adults, the diagnosis of which not rarely is a challenging task. The most common cause of PAD is atherosclerosis while there are other less common causes including vasculitis, dysplastic syndromes, degenerative conditions, thrombosis, and thromboembolism 1 . Atherosclerotic lower extremity PAD is characterized by intermittent claudication; this symptom manifests in only 10% of patients. 50% of patients have a variety of leg symptoms other than classic claudication, and 40% have no leg symptoms at all.2 The latter constellation pertains to higher morbidity and mortality and higher rates of lower
limb amputation, due to delayed detection. Therefore, it is of utmost importance to recognize the signs of early PAD and treat these patients accordingly. One of the main diagnostic methods used to assess the hemodynamic status of lower limbs and diagnose PAD is the ankle-brachial index (ABI). According to that, an ABI of 1.0-1.3 is considered normal, 0.9-1 borderline, 0.7-0.9 mild, 0.4-0.7 moderate and below 0.4 is defined as severe PAD.
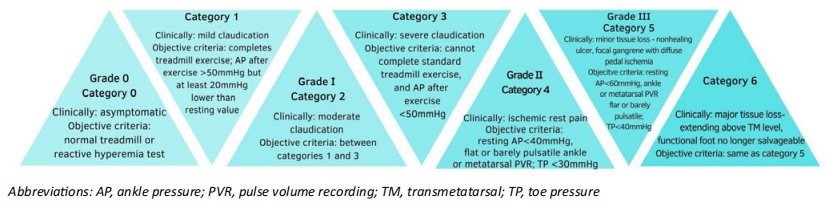
There are several classification systems for categorizing people with PAD based on disease severity and symptoms. The first classification system created was the Fontaine Classification that grades patients in 4 stages, based on clinical symptoms only. This classification is no longer used in clinical settings. The Rutherford classification system is the one which is widely used today. It does not solemnly describe the clinical presentation of the patient, but also includes laboratory and imaging findings like ABI, pulse volume recordings and Doppler ultrasound findings.
Figure 1. Rutherford classification for chronic limb ischemia 3
3.The complications of PAD, particularly in patients with DM have given rise to another classification system, i.e. WIFI (Wound, Ischemia, Foot infection) score from SVS (Society for Vascular Surgery). People are classified into five stages according to the risk of lower limb amputation. The following symptoms are considered: wounds, ischemia and foot infection, the severity of which is categorized on a scale between 0 and 3, with 0 representing absence of the respective symptom, 1 indicating mild manifestation of the symptom, 2 moderate-, and 3 severe manifestations. Following grading, the scores assigned to each symptom are pooled and assessed using two tables. The first provides an estimate of the risk of amputation at 1 year and the second an estimate of the necessity and potential benefit of revascularization. Based on the findings, the limb is categorized as having a very low, low, moderate, or high risk of amputation or potential benefit from revascularization at clinical stages 1, 2, 3, or 4, accordingly. Stage 5 is
only for irreparably damaged limbs that cannot be salvaged even with revascularization.4 Finally, it is important to note the current trends in limb amputation, where there is an increase in minor lower extremity amputation rates and a concurrent drop in major lower extremity amputation. These, along with the rise in patients’ age, may indicate a shift in the treatment of PAD. 5 However, significant psychological distress can result from even small partial amputations of single digits. Therefore it is important to effectively address complications like neuromas and provide psychological support services in the post-amputation period 6The complications of PAD, particularly in patients with DM have given rise to another classification system, i.e. WIFI (Wound, Ischemia, Foot infection) score from SVS (Society for Vascular Surgery). People are classified into five stages according to the risk of lower limb amputation. The following symptoms are considered: wounds, ischemia and foot infection, the severity of which is categorized on a scale between 0 and 3, with 0 representing absence of the respective symptom, 1 indicating mild manifestation of the symptom, 2 moderate-, and 3 severe manifestations. Following grading, the scores assigned to each symptom are pooled and assessed using two tables. The first provides an estimate of the risk of amputation at 1 year and the second an estimate of the necessity and potential benefit of revascularization. Based on the findings, the limb is categorized as having a very low, low, moderate, or high risk of amputation or potential benefit from revascularization at clinical stages 1, 2, 3, or 4, accordingly. Stage 5 is only for irreparably damaged limbs that cannot be salvaged even with revascularization.4 Finally, it is important to note the current trends in limb amputation, where there is an increase in minor lower extremity amputation rates and a concurrent drop in major lower extremity amputation. These, along with the rise in patients’ age, may indicate a shift in the treatment of PAD. 5 However, significant psychological distress can result from even small partial amputations of single digits. Therefore it is important to effectively address complications like neuromas and provide psychological support services in the post-amputation period 6
METHODS
This review was conducted using the databases PubMed and Google Scholar and articles were included up until November 2022. The selection of articles was based on a combination of the search terms “PAD”, “Psychiatric diseases”, “vascular diseases”, “diabetes”, “anxiety”, “depression”, “psychological status” and “amputation”. The articles that were generated from this search were then filtered to include peer-reviewed studies with sufficient sample sizes and valid study designs that had as their central objective the study of the association between vascular diseases and psychiatric symptoms. Exclusion criteria included duplicate studies, studies with insufficient numbers of patients, articles that were not written in English and studies that diverged from the main purpose of this review. Any disagreements over inclusion criteria were resolved by an independent Reviewer.
RESULTS
Mental illness symptoms Previous studies have shed light on the not rare coexistence of vascular diseases and mental illness symptoms. Patients with DM and complications such as ulcers and limb amputations report an overall lower quality of life and more depressive symptoms compared to people with DM but no complications7 . Part of this problem stems from the inadequate health education and awareness of patients regarding the process of amputation, particularly in lower-middle income countries. As a result, the perceptions of patients that need to undergo amputation are centered around the feeling of fear and anxiety over their altered self-image and social acceptance after
amputation. In fact, most of these patients tend to experience the stages of grief during this stage of their disease8 . Interestingly, a review of the psychological effects of amputation: reported depressive symptoms in 10.4-63% of patients and posttraumatic stress disorder (PTSD) in 3.3%-56.3% of amputees9 . Most studies report depressive symptoms as the most common mental illness symptoms in amputees, followed by anxiety symptoms 10.
It is important to note that there are reported differences in mental illness symptom frequency based on the cause of the amputation, with depression being particularly common among PVD-caused amputations and anxiety being more common in trauma-related amputations11. The strong association between traumatic injury amputation and PTSD has many implications for the mental and physical health of these patients. One notable effect is the high rate of substance misuse which includes problematic alcohol use, prescription medication overuse and illicit drug use among these patients. This link between substance abuse and PTSD further highlights the need for psychological assessment of these patients when deciding on an optimal treatment plan12.
Mental illness symptoms in people with PAD have shortand long-term effects. Depression, being the most common mental illness in people with PAD, has been shown to be associated with poor functional and surgical outcomes in PAD13 , even though the directionality and specific mechanisms underlying this relationship have not been thoroughly studied yet. In addition, depression in older adults is coupled with the presence of cognitive deficits 14, while a solid basis of evidence points to the high risk that late-onset depression confers for the development of dementia 15 through inflammatory, vascular and neurodegenerative processes 16. Moreover, higher levels of depression and anxiety pertain to worse quality of life17 and may act synergistically in potentiating the negative impact of PVD on quality of life.
Finally, cognition is also altered by amputation. These changes can be measured by the cognitive load or the mental resources required for task completion and information processing. The cognitive load of an amputee is significantly altered due to the changes in neuronal pathways, the effects of the phantom limb and the emotional changes that take place as a result of the amputation. Therefore, one study concluded that the standard components of the cognitive load should be extended when applying it to amputees to also include emotional and neural fatigue. These two elements include the emotional response to the amputation and the prosthesis, the concentration required to perform everyday tasks, as well as the altered proprioception and neuronal connections and the phantom phenomenon. Measuring the cognitive load has important clinical implications as it could be used to assess the adjustment of the patient to the prosthesis and aid in the best rehabilitation and psychological management post-amputation in order for the patient to achieve a low cognitive load state while performing everyday activities18.
Is there a need for mental health liaison services for people with PAD? Detecting and treating mental illness symptoms in patients with PAD (with amputation or even without) is of paramount importance. The high prevalence of mental illness symptoms in PVD and the serious risk of inducing further morbidity, they confer, highlights the importance of mental health liaison services for these patients within the frames of primary, secondary and tertiary prevention strategies. Nevertheless, very few studies have been performed to date that include a sufficient number of patients and enough follow-up time to be able to assess the potential benefits of such services in patients with PAD. One such study, which included one hundred newly amputated soldiers, found that a combination of medications and psychotherapy resulted in high rates of remission, with 62% of amputees with major depression achieving complete recovery11. Further, larger studies that include patients in different stages of the disease course are urgently needed in order to establish the best approach and time point of intervention.
CONCLUSION
Mental illness is a common comorbidity in PAD. Although mounting research evidence points to a significant prevalence of mental illness symptoms in PAD and their impact in disease course and management and the quality of life of patients, the awareness among experts in vascular surgery seems to be relatively low so far. Large-scale multidisciplinary studies are needed in order to develop adequate strategies to manage such symptoms and improve quality of life of patients.
References
1 Conte SM, Vale PR. Peripheral Arterial Disease. Heart Lung Circ. 2018;27(4):427-432. doi:10.1016/j.hlc.2017.10.014
2 Firnhaber JM, Powell CS. Lower Extremity Peripheral Artery Disease: Diagnosis and Treatment. Am Fam Physician. 2019;99(6):362-369.
3 Hardman R, Jazaeri O, Yi J, Smith M, Gupta R. Overview of Classification Systems in Peripheral Artery Disease. Semin Interv Radiol. 2014;31(04):378-388. doi:10.1055/s-0034-1393976
4 Cerqueira L de O, Duarte Júnior EG, Barros AL de S, Cerqueira JR, Araújo WJB de. Classificação WifI: o novo sistema de classificação da Society for Vascular Surgery paramembros inferiores ameaçados, uma revisão de literatura. J Vasc Bras. 2020;19:e20190070. doi:10.1590/1677-5449.190070
5 Essien SK, Kopriva D, Linassi AG, Zucker-Levin A. Trends of limb amputation considering type, level, sex and age in Saskatchewan, Canada 2006-2019: an in-depth assessment. Arch Public Health. 2022;80(1):10. doi:10.1186/s13690-021-00759-1
6 Skoff H, Skoff H. The Psychological and Somatic Consequences of Digital Amputation. Plast Reconstr Surg – Glob Open. 2022;10(6):e4387. doi:10.1097/GOX.0000000000004387
7 Carrington AL, Mawdsley SKV, Morley M, Kincey J, Boulton AJM. Psychological status of diabetic people with or without lower limb disability. Diabetes Res Clin Pract. 1996;32(1-2):19-25. doi:10.1016/0168-8227(96)01198-9
8 Owolabi EO, Chu KM. Knowledge, attitude and perception towards lower limb amputation amongst persons living with diabetes in rural South Africa: A qualitative study. Afr J Prim Health Care Fam Med. 2022;14(1). doi:10.4102/ phcfm.v14i1.3398
9 Sahu A, Sagar R, Sarkar S, Sagar S. Psychological effects of amputation: A review of studies from India. Ind Psychiatry J. 2016;25(1):4. doi:10.4103/0972-6748.196041
10 Shukla GD, Sahu SC, Tripathi RP, Gupta DK. A Psychiatric Study of Amputees. Br J Psychiatry. 1982;141(1):50-53. doi:10.1192/bjp.141.1.50
11 Baby S, Chaudhury S, Walia T. Evaluation of treatment of psychiatric morbidity among limb amputees. Ind Psychiatry J. 2018;27(2):240. doi:10.4103/ipj.ipj_69_18
12 Kearns NT, Powers MB, Jackson WT, Elliott TR, Ryan T. Post traumatic stress disorder symptom clusters and substance use among patients with upper limb amputations due to traumatic injury. Disabil Rehabil. 2019;41(26):3157-3164. doi:10.1080/09638288.2018.1485180
13 Ramirez JL, Drudi LM, Grenon SM. Review of biologic and behavioral risk factors linking depression and peripheral artery disease. Vasc Med. 2018;23(5):478-488. doi:10.1177/1358863X18773161
14 Alexopoulos GS. Mechanisms and treatment of late life depression. Transl Psychiatry. 2019;9(1):188. 138 Hellenic Journal of Vascular and Endovascular Surgery | Volume 4 – Issue 4 – 2022 doi:10.1038/s41398-019-0514-6
15 Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention, intervention, and care. The Lancet. 2017;390(10113):2673-2734. doi:10.1016/S0140-6736(17)31363-6
16 Hakim AM. Depression, Strokes and Dementia: New Biological Insights into an Unfortunate Pathway. Cardiovasc Psychiatry Neurol. 2011;2011:1-6. doi:10.1155/2011/649629
17 Ribeiro O, Teixeira L, Araújo L, Rodríguez-Blázquez C, Calderón-Larrañaga A, Forjaz MJ. Anxiety, Depression and Quality of Life in Older Adults: Trajectories of Influence across Age. Int J Environ Res Public Health. 2020;17(23):9039. doi:10.3390/ijerph17239039
18 Rackerby R, Lukosch S, Munro D. Understanding and Measuring the Cognitive Load of Amputees for Rehabilitation and Prosthesis Development. Arch Rehabil Res Clin Transl. 2022;4(3):100216. doi:10.1016/j.arrct.2022.100216


