Lessons learned from a case of complicated type II endoleak: when endograft explantation is the only solution

| Available Online: | May, 2023 |
| Page: | 13-16 |
*Author for correspondence:
Giovanni Mastrangelo
n°23, Contrada Piano strada n°5, San Giovanni Rotondo (FG), 71013, Italy
E-mail: giovanni.mastrangelo.86@gmail.com
doi: 10.59037/hjves.v5i1.34
ISSN 2732-7175 / 2023 Hellenic Society of Vascular and Endovascular Surgery Published by Rotonda Publications
All rights reserved. https://www.heljves.com
Giovanni Mastrangelo1,2, Federico Pascucci1,3, Giancarlo Palena1, Vincenzo Sciannelli1, Gabriele Magistro1, Roberto Marinucci1, Luigi Semerano1, Vincenzo Palazzo1
1 Unit of Vascular Surgery, Fondazione IRCCS Casa Sollievo della Sofferenza, San Giovanni Rotondo (FG), 71013, Italy
2 Department of Innovative Technologies in Medicine & Dentistry, University “G. d’Annunzio” Chieti-Pescara, 66100 Chieti, Italy
3 Vascular Surgery Residency Program, Fondazione Policlinico Universitario Gemelli IRCCS-Università Cattolica del Sacro Cuore, Largo Agostino Gemelli, 8, 00168 Rome, Italy.
Abstract
Full Text
References
Images
Abstract
We report the case of a 69-year-old man with a computed tomography angiography (CTA) scan showing an abdominal aortic aneurysm with a bifurcated endograft and a type II endoleak. Our first strategy was the embolization of the inferior mesenteric artery with coils, via superior mesenteric artery and marginal colic artery; then we made another endovascular attempt to reach the T2EL with the transarterial technique but without success. After a multisciplinary consultation, we decided to resort to open conversion. Sacotomy revealed that the aneurysm was being supplied posteriorly, from the infrarenal sealing zone of the endograft (unknown type IA endoleak). Thus, we removed the stent-graft and performed an aorto-bifemoral bypass surgery. From this case we learned two lessons: all possible causes of relapsing and complicated type II endoleak should be investigated (also with CEUS or MRI), and open repair surgery (including endograft explantation) should not be considered only as a last resort in patients fit for surgery.
Keywords: Type II endoleak, open conversion; sac growth, embolization, EVAR.
Full Text
INTRODUCTION
With the introduction of the endovascular aortic repair (EVAR) procedure, the treatment of abdominal aortic aneurysm has deeply changed in the last 30 years1. However, EVAR has recently been shown to be associated with higher rates of long-term complications and need for reintervention2. Most of these reinterventions are due to endoleaks (EL) which occur in up to 20% of all EVAR procedures3. The type II endoleak (T2EL) represents one of the most common complications. In this case report, we describe all the techniques that we applied in our center to treat a complicated T2EL.
CASE REPORT
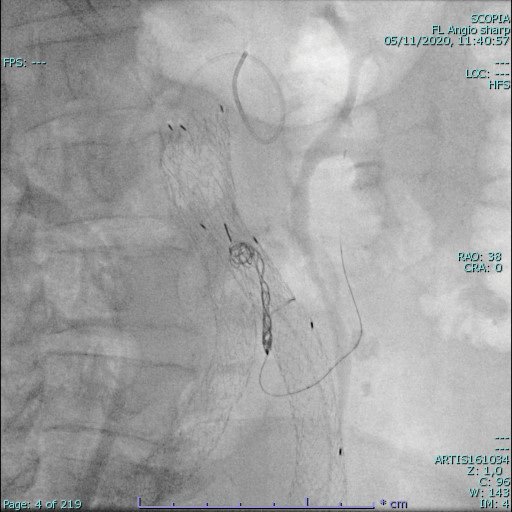
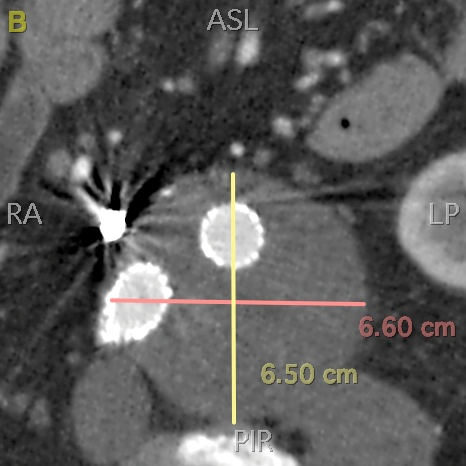
We report the case of a 69-year-old man with a history of hypertension and EVAR, performed in another Hospital two years before with a bifurcated Excluder abdominal aortic endoprosthesis (GW.L. Gore & Associates, Flagstaff, Ariz) for an abdominal aortic aneurysm. Computed tomography angiography showed an increased aneurysm sac diameter, from 48 mm at the last CTA in 2019 to 54 mm, and a suspected T2EL from the inferior mesenteric artery (IMA) . Our first strategy was the embolization of the IMA : with a 6 F Simmond catheter, through a left femoral access, we reached the superior mesenteric artery ostium and, on a 0.014” hydrophilic guidewire (Avigo, Medtronic Inc, Swinnea), via the superior mesenteric artery, the middle colic and the marginal artery of the colon (of Drummonds), using a pre-shaped microcatheter (145-5091-150 Echelon 10) we embolized the first segment of the IMA with coils (Axium coils, diameters from 8 to 3.5 mm) (fig.1). We decided to limit our intervention to IMA embolization. Three months after, the CTA showed that the IMA was successfully embolized, but it also showed a slight increase of the aneurysmal left iliac-aortic sac (59 mm diameter), with an increasing lumbar arteries (LA) type II endoleak. Thus, we decided to use a second endovascular approach: from a right femoral access, via transiliac paraendograft4 we attempted to make the endoleak embolization, but without success because of the complete adhesion of the limb to the iliac wall. In addition, we tried to embolize the culprit LA through the catheterization of the internal iliac and iliolumbar arteries, but the anastomosis webs were too small to be navigated. After three months we found an evident posterior type II endoleak (66mm x 60 mm new sac diameter). Together with the general surgeon and the interventional radiologist, we decided to convert to open repair through midline laparotomy, surgical ligation of extra-aneurysmal backbleeders, sacotomy via a longitudinal aortotomy, endoaneurysmorrhaphy, and stent-graft preservation. After sacotomy, we discovered that the aneurysm sac was being supplied posteriorly, from the infrarenal sealing zone of the endograft. Proximal and distal control was obtained by cross-clamping the aorta and the iliac arteries. Finally, we removed the stent-graft (fig.2) and performed an aorto-bifemoral bypass procedure. Then the patient was sent to the Intensive Care Unit for 72 hours and discharged at the 8th post-operative day with the single anti-aggregation therapy. The 1-month-follow-up CTA showed that the endoleak had been successfully corrected by surgery and that the graft had a good patency, also confirmed by the 6-month-follow-up US scan (fig.3).
DISCUSSION
The 2019 European Society for Vascular and Endovascular Surgery (ESVS) guidelines reported that an expansion of sac diameter of at least 1 cm (a significant growth), detected during the follow-up after endovascular abdominal aortic aneurysm repair using the imaging modality and the measurement method, should be considered for the treatment. A recent systematic review has shown that T2EL after EVAR has a pooled prevalence of 22%, with a reintervention rate of 19%5. In addition, EVAR has been reported6 to be associated with the following features: 1. after EVAR the access to the IMA or LA may be limited; and 2. the recurrence rate of T2EL after an endovascular treatment ranges from 25-80%.
A wide range of treatment options exist, including transarterial embolization, percutaneous direct sac puncture embolization, transcaval embolization, conservative and surgical management7. The failure of conservative and endovascular strategies for the treatment of a persistently enlarging T2EL-associated aneurysm is rare, but it requires a surgical approach (tab.1). One of these could be laparoscopy: it remains a technically challenging procedure because of the inflammation of the sac after EVAR. This strategy is not frequently applied because it is possible in few and selected centers where there are specifically trained vascular surgeons (often in collaboration with specifically trained general surgeons)8,9. Another approach is the obliterating endoaneurysmorrhaphy with in situ preservation of the endograft, which was our first plan for the open surgery solution. Furthermore, since some studies8,10 have reported that some relapsing T2ELs were associated with a different type of endoleak which was missed on the preoperative CTA and since, as we report in tab.1, patients with an occult endoleak may be particularly difficult to manage with the endovascular therapy, we believe an earlier consideration of open surgery (graft explantation included) for patients with an acceptable surgical risk should be advisable. The lessons that we learned with this challenging case of a patient fit for surgery are that: 1. all possible causes of relapsing and complicated type II endoleak should be investigated (also with CEUS or MRI); 2. open surgery represents a good strategy to treat a persistent and relapsing T2EL with an enlarging aneurysm sac. The circumstances which cause the occult endoleak to develop are still unclear. 10
CONCLUSION
The technical success of open repair surgery on our fit-for-surgery patient confirms that this strategy could be a solution in relapsing and complicated T2ELs. The open surgery strategy should be taken into consideration also for persistent T2EL because it may hide other types of endoleak. Other investigators10 have recommended the use of alternative diagnostic modalities, such as contrasted-enhanced ultrasound imaging (which should only be performed by experienced angiologists) combined with CTA or pooled magnetic resonance imaging, as effective supporting tools in the detection of occult endoleaks.
ACKNOWLEDGEMENTS
We would like to thank Chiara Di Giorgio (Fondazione IRCCS Casa Sollievo della Sofferenza) for editing and reviewing this manuscript for English language.
Table 1: Literature review
|
Study |
Type of study |
|
Ken Min Chin et al. |
Case-report |
|
Pierre Maitrias et al. |
Observational study |
|
Madigan MC et al. |
Retrospective study |
|
Aziz A, et al. |
Retrospective study |
References
- Ivancev K, Vogelzang R. A 35 Year History of Stent Grafting, and How EVAR Conquered the World. Eur J Vasc Endovasc Surg 2020;59:685-694.
- Chin KM, Lee SQW, Lee HJ, Ping CS, Chng JK. Preservation of Stent Graft after Iatrogenic Type III Endoleak during Open Transperitoneal Surgical Intervention for Complicated Type II Endoleak. Ann Vasc Surg 2019;1.e1-1.e7.
- Prinssen M, Verhoeven EL, Buth J, Cuypers PW, van Sambeek MR, Balm R, et al; Dutch Randomized Endovascular Aneurysm Management (DREAM) Trial Group. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med 2004;351:1607-18.
- Ameli-Renani S, Pavlidis V, Mailli L, Turner P, Morga RA. Transiliac Paraendograft Embolisation of Type 2 Endoleak: An Alternative Approach for Endoleak Management. Cardiovasc Intervent Radiol 2016;39:279-283.
- Qiang G, Xiaojiong D, Jichun Z, Yukui M, Bin H, Ding Y, et al. Prevalence and risk factors of type II endoleaks after endovascular aneurysm repair: A meta-analysis. PLoS One 2017;12:e0170600.
- Hajibandeh S, Ahmad N, Antoniou GA, Torella F. Is intervention better than surveillance in patients with type 2 endoleak post-endovascular abdominal aortic aneurysm repair? Interact Cardiovasc Thorac Surg 2015;20:128-34.
- Grima MJ, Karthikesalingam A. Type II endoleaks: when and how, The Journal of Cardiovascular surgery 2017;58:889-94.
- Maitrias P, Kaladji A, Plissonnier D, Amiot S, Sabatier J, Coggia M, et al. Treatment of sac expansion after endovascular aneurysm repair with obliterating endoaneurysmorrhaphy and stent graft preservation. J Vasc Surg 2016;63:902-8.
- Wee I, Marjot T, Patel K, Bhrugubanda V, Choong AMTL. Laparoscopic ligation of Type II endoleaks following endovascular aneurysm repair: A systematic review. Vascular 2018;26:657-669.
- Madigan MC, Singh MJ, Chaer RA, Al-Khoury GE, Makaroun MS. Occult type I or III endoleaks are a common cause of failure of type II endoleak treatment after endovascular aortic repair. J Vasc Surg 2019;69:432-439.