Acute upper limb ischemia in a patient recently vaccinated for Covid-19

| Available Online: | April, 2023 |
| Page: | 143-145 |
Author for correspondence:
Simlawo Kpatékana
University Hospital center of Sylvanus Olympio, Togo
E-mail: Richardsim82@yahoo.fr
doi: 10.59037/hjves.v4i4.10
ISSN 2732-7175 / 2022 Hellenic Society of Vascular and Endovascular Surgery Published by Rotonda Publications
All rights reserved. https://www.heljves.com
Simlawo Kpatékana1 , Sanvi Kossi Arsène Elvis1 , Pio Machihude2 , Fortey Yawo Hervé3 , Coppin Thierry3 , Dosseh Ekoué David1
1 University Hospital center of Sylvanus Olympio, Togo
2 University Hospital center of Kara, Togo
3 Hospital center of Douai, France
Abstract
Full Text
References
Abstract
Vascular complications of Covid-19 disease represent significant causes of morbidity and mortality, being both life- and limb-threatening. Although extremely rarely, the various vaccines against Covid-19 infection have also been associated with thromboembolic complications. We describe a patient who presented with right upper limb acute ischemia three days after her vaccination and who had a positive PCR test. Thrombosis of the axillary artery was revealed by computed tomography angiography and the patient was submitted to thrombectomy with complete restoration of upper limb perfusion. We also review the recommendations of scientific societies on the management of acute limb ischemia in the particular etiological context of Covid-19.
Keywords: Acute, Ischemia, Limb, Covid-19, Vaccine.
Full Text
INTRODUCTION
Vascular complications of Covid-19 disease represent significant causes of morbidity and mortality, being both life- and limb-threatening, in cases of acute limb ischemia (ALI).1 Although much less frequently, vascular complications have also been described after Covid-19 vaccination, causing the population to be skeptical of vaccines. Herein we describe a patient who presented with right upper limb acute ischemia three days after her vaccination and who, at the same time, had a positive PCR test at her admission. The cause of ischemia in this patient was unclear: was it the covid-19 infection or the Covid-19 vaccine? The second objective of this study was to analyse the recommendations of scientific societies on the management of ALI in the particular etiological context of Covid-19.
OBSERVATION
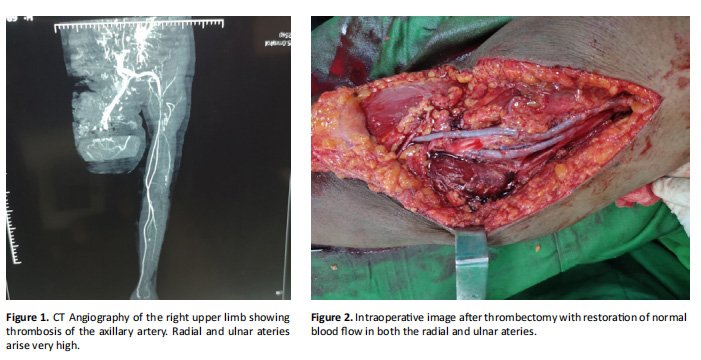
A 55-year-old female presented to our hospital with acute upper limb ischemia. She was hypertensive under treatment, with no history of heart disease. She had been vaccinated with the Janssen (Johnson & Johnson) COVID-19 vaccine and had suffered from headaches, within the following 24 hours. Three days after vaccination, she experienced disabling pain in her right upper limb, with partial loss of motor function. On physical examination, the limb was cold and with no palpable pulse at the right axillary, brachial, radial and ulnar artery. There was paraesthesia of the right hand. Lab tests revealed a CRP of 27.45 mg/L, a neutrophil count of 6,600/μl and lymphocyte count of 2,000/μl. There was monocytosis of 1,400/ μl and an Erythrocyte Sedimentation Rate (ESR) of 95. The patient underwent a Computed Tomography Angiography (CTA) revealing thrombosis of the right axillary artery extending to the brachial artery (Figure 1). The patient was started on unfractionated heparin and was taken to the operating room where an incision crossing the elbow crease was performed and both the radial and the ulnar artery were exposed, since the bifurcation of the brachial artery was very high at the level of the axilla. Thrombectomy of the axillary, brachial, radial and ulnar arteries with the use of a Fogarty catheter followed (Figure 1). At the end of the procedure, there was a very good reperfusion of the radial and ulnar arteries (Figure 2), verifying the patency of the inflow arteries. Palpable pulse of both the ulnar and the radial artery at the level of the wrist was restored. The patient was started on rivaroxaban 20 mg od and had an uneventful postoperative course. At the last follow-up visit, six months later, the patient remained asymptomatic and the anticoagulants were discontinued. Cardiac tests, including Holter ECG and Doppler echocardiography revealed no embologenic heart disease.
DISCUSSION
Arterial thromboembolism is a rare complication of Covid-19 disease. In a large retrospective, multicenter study performed in California from March 2020 to March 2021, the incidence of arterial thromboembolism was found to be 0.07%.2 Upper limb arterial thromboembolism is even less common, and the few publications in the literature are limited to reports of a single case.1 Arterial thromboembolism after vaccination against Covid-19 is extremely rare.3 ALI can be a complication of pre-existing peripheral arterial disease with thrombus formation on a plaque and subsequent distal embolism. It can also occur in a healthy artery as in our patient. Differential diagnosis included cardiogenic embolism or in situ thrombosis,4,5 which was probably the case in our patient, as evidenced by the normal cardiac assessment, including a normal echocardiography, and the results of the CT angiography showing the absence of a collateral network (Figure 1). The cause of the ischemia in our patient may be the Covid-19 infection. Indeed, in Covid-19 disease, haematological changes occur leading to hypercoagulability.
Biological analyses of the blood of patients with Covid-19 show a low level of antithrombin and high levels of D-dimers, fibrinogen and fibrin/fibrinogen degradation products with a statistically significant difference from controls.6 Oxidative stress plays a very important role, with a combination of neutrophilia and lymphopenia, elevation of CRP and reactive oxygen species (ROS) causing endothelial cell dysfunction and platelet augmentation and aggregation, resulting in clot formation.7 Thrombus and the resulting ischemia can also be a rare complication of the vaccine. This could be the case in our patient. Most, if not all, Covid-19 vaccines are associated with thromboembolic complications as side effects, including the Jansen vaccine. Its involvement in the occurrence of rare thromboembolic events has been established by numerous publications and accepted by the European Medicines Agency.8,9 The accepted mechanism in the genesis of these thromboses is vaccine-induced immune thrombotic thrombocytopenia (VITT), involving anti-platelet factor IgG mimicking the mechanism of Heparin-Induced Thrombocytopenia (HIT). Apart from immunological assays, several criteria make it possible to make the diagnosis of VITT, including vaccination against Covid-19, recent thrombocytopenia, no previous exposure to unfractionated heparins and no other explanation for thrombocytopenia.9 Another, theoretical, explanation for the thromboembolism in our patient could be the joint action on the coagulation system of both the Covid-19 progressive infection and the recent vaccination. It has to be noted that this theory is hypothetical since there is no evidence in the literature of this mechanism neither do we have sufficient proof to support it. Yet, this is suspected due to the coincidence of the Covid-19 disease and the vaccination. The management of acute limb ischemia is fairly well established by the various scientific societies for vascular surgery. According to the recommendations of the ESVS,10 as soon as the diagnosis is made and awaiting operative management, if indicated, heparin is recommended by consensus. Surgical management is performed in a hydrid room with angiographic evaluation of the result at the end of the procedure.10 Due to the lack of specific guidelines for the treatment of acute limb ischemia caused by Covid-19, these guidelines should be extended to the Covid-19 patients as well. In our case, success of the thrombectomy was verified by the resumption of adequate arterial inflow and also by the restoration of distal pulsPostoperatively, the color and the temperature of the limb were restored to normal, the neurological signs disappeared and the arterial Doppler ultrasound signals were normal.
CONCLUSION
Acute ischemia of the upper limb is a very rare complication of covid-19 infection and an even rarer side effect of covid-19 vaccination. When it occurs in a person who is recently vaccinated against covid-19 disease and who was already infected by coronavirus disease without knowing, it is questionable whether the cause of the arterial thromboembolism is the Covid-19 disease, the vaccine or the combination of both. Further studies are needed to clarify this issue.
References
1 Bellosta R, Luzzani L, Natalini G, Pegorer M A, Attisani L, Cossu L G, et al. Acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg 2020;72:1864-1872.
2 Vo TD, Daoud A, Jeney A, Andacheh I, Behseresht J, Hsu J, et al. COVID-19-related Peripheral Arterial Thrombosis Treated in a Large Health Maintenance Organization. Ann Vasc Surg 2022;22:S0890-5096(22)00208-4.
3 Jones M, Boisvert A, Landry J, Petrasek PF. Ischémie d’un membre et thrombose de l’artère pulmonaire après l’administration du vaccin ChAdOx1 nCoV-19 (Oxford-AstraZeneca): un cas de thrombocytopénie thrombotique immunitaire induite par le vaccin. CMAJ 2021;193:1021-
4 Coscas R, Boura B, Koskas F, Julia P, Fabiani J-N. Ischémie aiguë de membre. EMC (Elsevier Masson SAS, Paris), Angéiologie 2009;19-0530.
5 Schneider F, Ricco JB. Ischémie aiguë des membres inférieurs. EMC; Techniques chirurgicales- Chirurgie vasculaire, 2015, 43-028-H.
6 Han H, Yang L, Liu R, Liu F, Wu K, Li J, et al. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. CCLM 2020; 58:1116-1120.
7 Laforge M, Elbim C, Fr`ere C, H´emadi M, Massaad C, Nuss P et al. Tissue damage from neutrophil-induced oxidative stress in COVID-19, Nat Rev Immunol 2020;20:515-516.
8 Yann-Mickael Dalmat. Thrombose cérébrale après vaccination. Option/Bio. 2021;32:12.
9 Mayte Sánchez van Kammen, Diana Aguiar de Sousa, Sven Poli, Charlotte Cordonnier, Mirjam R Heldner, Anita van de Munckhof, et al. Characteristics and Outcomes of Patients With Cerebral Venous Sinus Thrombosis in SARSCoV-2 Vaccine-Induced Immune Thrombotic Thrombocytopenia. JAMA Neurol 2021;78:1314-1323.10 Björck M, Earnshaw JJ, Acosta S, Bastos Gonçalves F, Cochennec F, Debus ES, Hinchliffe R, Jongkind V et al. Clinical Practice Guidelines on the Management of Acute Limb Ischaemia. Eur J Vasc Endovasc Surg 2020;59:173-218.


