Acute carotid stent thrombosis (ACST): a review study

| Available Online: | October, 2023 |
| Page: | 132-138 |
Author for correspondence:
Anastasia K. Kouri
School of Medicine, Department of Vascular Surgery, University Hospital of Patras, Greece, Rion, Achaia, 26504
Τel: +30 6948380805
E-mail: natasa.kouri@gmail.com
doi: 10.59037/nyv9m480
ISSN 2732-7175 / 2023 Hellenic Society of Vascular and Endovascular Surgery Published by Rotonda Publications All rights reserved. https://www.heljves.com
Abstract
Full Text
References
Images
Abstract
Abstract:
Objective: Acute carotid stent thrombosis (ACST) is a rare complication of carotid artery stenting (CAS), occurring within 30 days after CAS and can lead to devastating, even lethal consequences. The purpose of this study is to review the current literature on ACST and investigate the potential causative factors and the available therapeutic strategies.
Methods: A search of multiple electronic health databases was conducted. A total of 37 cases reporting acute ACST were retrieved.
Results: There were 33 male and 4 female patients [mean age 68.54 years (SD ±7.98 y)]. 21.62% (8 cases) referred to asymptomatic carotid stenosis. The left internal carotid artery (ICA) was the predominant site of carotid stenosis (24/37 cases, 64.86%). In 13(35.1%) of cases ACST occurred intra procedurally, in 10 (27%) within the first 24 hours, in 13 (35.1%) within the first week after CAS. In 1 (2.7%) case there was late thrombosis 3 weeks after CAS. Inadequate antiplatelet therapy, thrombotic predisposition, or antiplatelet resistance, were described as possible causes in 42.3% of cases. The most common technical intraprocedural anatomic causes leading to ACST were ICA dissection, overlapping stents, plaque protrusion along the stent, and thrombosis of embolic protection devices (EPDs). Treatment varied according to the time of carotid stent thrombosis, the cause, and the patient’s neurologic status. Antiplatelet therapy in combination with antithrombotic agents (heparin, warfarin, argatroban), intravenous infusion of platelet glycoprotein IIb/IIIa inhibitors (GPIs), thrombolysis, mechanical thrombectomy, thromboaspiration with thrombolysis, open surgery and re angioplasty were reported as therapeutic strategies. In the majority of cases clinical improvement with resolution of neurological symptoms or residual neurological deficit was observed. Two deaths (5.4%) were reported.
Conclusion: Although, there is no consensus regarding the management of ACST, thrombolysis, mechanical thrombectomy, thromboaspiration with thrombolysis, open surgery and re-angioplasty have all been used with promising results. The critical points for preventing the devastating outcome are immediate recognition of the thrombosis and rapid revascularization of the damaged tissue.
Keywords: Carotid stent; acute thrombosis; stroke; revascularization
Full Text
INTRODUCTION
Acute carotid stent thrombosis is a rare complication of carotid artery stenting (CAS), the prevalence of which varies between 0.5% to 0.8%.1 It is a devastating complication that can lead to a stroke and death and occurs within 30 days after CAS.1-4 This serious complication requires early diagnosis and prompt restoration of cerebral perfusion via internal carotid artery (ICA) recanalization to limit ischemic brain damage.5 There are several case reports in the literature, but no large series and there are no specific guidelines regarding the ideal strategy for treating ACST. The purpose of this study is to review the current literature on this devastating complication occurring after CAS to investigate potential etiological factors and to explore available therapeutic strategies and outcomes of treated patients.
METHODS
A multiple search of electronic health databases, including MEDLINE/PUBMED and EMBASE, was performed for all articles published up to June 2022 on carotid stent thrombosis after CAS. Only cases with ACST were included in our study. ACST was defined as those thromboses occurring in the first hours or days after the procedure. Late thromboses (> 30days after CAS) were excluded from the study.
Search strategy
Studies were identified by searching electronic databases and scanning bibliographic references of articles. The National Library of Medicine’s Medline database was searched using the PubMed interface and SCOPUS from through June 2022. No language constraints were used. Keywords were selected using medical subject headings (MeSH) for PubMed and MeSH/Emtree for Scopus. The keywords “acute”, “carotid stent”, and “thrombosis”, were used. Databases were searched with an unrestricted search strategy, applying exploded MeSH and keywords combined with the Boolean operator AND to retrieve relevant reports. A second-level search included a manual screen of the reference lists of the articles identified through the electronic search.
Age and sex, degree and location of stenosis, incidence, perioperative antiplatelet medication, cause of ACST, type of treatment, and outcome were retrieved and analyzed.
RESULTS
The search identified 277 records in total after applying the inclusion criteria. All studies were reviewed and a total of 25 studies, describing the outcome of 37 patients with ACST, met the inclusion criteria.1-3,6-9,11,13,15-30 The included studies were case reports and small series. In the present study, 33 out of 37 patients were male with a mean age of 68.54 years (SD ±7.98, min 44, max 82 y), and only 21.62% (8 cases) were treated with CAS for asymptomatic carotid stenosis. In the majority of cases (89.19%) mono or dual antiplatelet therapy was used pre-procedurally. The left internal carotid artery (LICA) was the predominant site of carotid stenosis (24/37 cases, 64,86%). In 13 (35.1%) cases ACST occurred intra procedurally, while in 10 (27%) patients, stent thrombosis occured within the first 24 hours. The remaining 13 (35.1%) cases reported ACST within the first week after CAS. In 1(2.7%) case there was a thrombosis 3 weeks after CAS. Overall, two deaths (5.4%) were reported.
Etiology
The cause of thrombosis was not defined in 11 out of the 37 cases (Table 1).
Inadequate antiplatelet therapy, thrombotic predisposition or antiplatelet resistance were described as possible causes in 11(42.3%) of cases (table 1). Three cases of hypercoagulation (3/26, 11.1%) were described due to malignancy 15,22,27 and one more was attributed to atrial fibrillation by Setacci et al.21
Technical intraprocedural anatomical causes which led to ACST were identified as follows: ICA dissection in 2 cases11, plaque protrusion across the stent in one patient27, overlapping stents in 3 cases (due to malposition in two of them and a long common carotid stenosis in one case)27, percutaneous transluminal angioplasty (PTA) failure in 3 reports11,20,25 and embolic protection devices (EPD) complications in 5 patients 1,16,24 (4 cases of EPD thrombosis and 1 case of ICA dissection). A combination of the abovementioned causes was reported in 4 cases (Table 1).
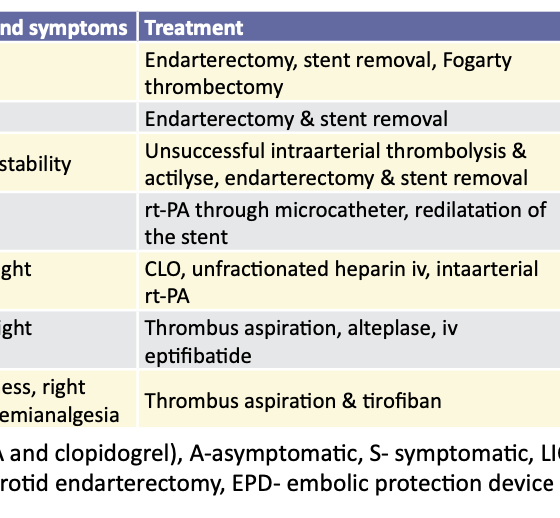
Therapeutic Management
Antiplatelet therapy in combination with antithrombotic agents
Eight patients were treated with antiplatelet therapy (single or dual) in combination with antithrombotic agents (low molecular weight heparin, warfarin, argatroban) or intravenous (IV) infusion of GPIs.8,15,25,26,27 Data on the use of GPIs are relatively limited, and fatal intracranial hemorrhage has been reported as a complication5. Abciximab was used alone or in combination with other thrombolytic agents and showed efficacy in dissolving an in-stent thrombus ( IV bolus dosage of 0.25mg/kg and a 0.125mg/kg intra-arterially, followed by IV infusion of 0.125mg/kg/min for further 12 hours).6,7,8
In the majority of cases, resolution of neurological symptoms or residual paresis was observed. In one case treated with aspirin alone, death occurred (Table 2).2
Thrombolysis ± Re-Angioplasty
In 12 patients thrombolysis was performed which was unsuccessful in 4 of them and further treatment was needed. Thrombolysis in patients with acute ischemic stroke attributed to ICA occlusion can be infused either intra-arterially or IV. Several thrombolytic agents such as streptokinase, urokinase, tenecteplase, or rtPA have been used for the treatment of acute ACST intra-arterially with complete, partial, or even unsuccessful clot resolution.2,7,10,11,12,13 A clinical improvement and a patent stent in the majority of cases were described (Table 2). Studies have recorded the beneficial effect of IV thrombolysis9,10, however, an increase in death and intracranial bleeding were also documented.6 In one case treated with urokinase, a death occurred (Table 2).2
3 cases were treated with re-angioplasty or stenting. Owens et al reported thrombolysis and repeat angioplasty, leading to ICA thrombosis and rupture.18 Masuo et al described an intraprocedural ACST treated with redo in stent PTA using an EPD, followed by intravenous heparin infusion for 7 days with a residual mild hemiparesis.19 Finally, Hu et al reported intraprocedural in stent thrombosis treated with microcatheter infusion of rt-PA and re-angioplasty.20
Mechanical thrombectomy or thromboaspiration with or without thrombolysis
8 patients underwent mechanical thrombectomy with or without thrombolysis. The Penumbra system showed promising results with complete recanalization and neurological improvement in 3 patients (Table 2).24 Thromboaspiration combined with thrombolysis or anticoagulants (abciximab) has shown clinical improvement and stent recanalization.16,17,28,30 It offers an alternative, however EPD occlusion has been reported.15,16 Dhall et al have reported complete patency restoration with the use of a thromboaspiration catheter before EPD withdrawal.17 Mechanical thrombectomy and stenting were associated with higher recanalization rates and improved functional status when compared to intra-arterial thrombolysis.12
Open Surgical Exploration
12 patients underwent surgical exploration (Table 2), due to described major neurological deterioration.1,13,18,21,23,29 Strategies such as carotid thromboendarterectomy and stent explantation, open surgical thrombectomy without stent removal, primary or patch closure, use of shunt or not, and even bypass from superficial temporal artery to middle cerebral artery (STA-MCA) were reported.
DISCUSSION
Acute carotid stent thrombosis remains a rare complication of CAS, occurring during or after less than 1% of procedures.1 According to the available literature, 37 cases reporting acute carotid stent thrombosis in the early period (<30 days) have been recognized. Many factors have been implicated as responsible for ACST. Our study showed that the predominant factors for carotid stent thrombosis are inadequate antiplatelet therapy, thrombotic predisposition, and the antiplatelet resistance.3 Furthermore, technical intraprocedural anatomical causes predisposing to carotid stent thrombosis are local vessel dissection or intimal injury leading to platelet adhesion and thus thrombus formation11,25, plaque protrusion promoting thrombosis, kinking and even coiling of the distal part of ICA27, vasospasm, stent underexpansion which impairs stent’s thombogenicity itself28, overlapping carotid stents27 and EPD occlusion.4,16,24 It is supported that EPD occlusion and carotid stent thrombosis are sequential events as they have been attributed to similar mechanisms.4,16,24
Our study showed heterogeneity in the type of treatment used, the severity of the patient’s neurological condition, and the extent of brain damage. In the majority of cases, clinical improvement was observed with a resolution of neurological symptoms or residual neurological deficit. Two deaths (5.4%) were reported. However, this rate might be underestimated by the fact that ACST cases with a fatal outcome may have been avoided for publication. Thrombolysis, mechanical thrombectomy, thromboaspiration with thrombolysis, open surgical therapy, and re-angioplasty have all been used, depending on the time of thrombosis, cause, and neurological status of the patient, with promising results. The main goal of ACST treatment is to promptly remove the source of thrombus to limit ischemia time, reperfusion injury, and potential post-procedure related intracranial hemorrhage.
Emergent removal of the thrombosed stent is indicated in ACST patients with immediate neurological deterioration, especially when the in-stent thrombosis is not associated with intracranial carotid branch thrombosis. The emergency operation has the risk of clot dislocation due to surgical maneuvers and therefore demands extended site exposure and careful preparation to protect distal cerebral embolization.1
Several studies have documented the beneficial effect of intra-arterial thrombolysis.2,6,7,9-13 It can be used rapidly especially when ACST occurs intraprocedurally. Although local intra-arterial thrombolysis might have a high recanalization rate, however, intraluminal manipulation of wires and catheters combined with thrombus lysis can cause clot fragmentation and therefore distal cerebral occlusion. The residual thrombus within the stent predisposes to restenosis or even re-thrombosis of the stent. Intra-arterial thrombolysis with redo PTA or stenting may be another alternative for treating ACST.18-20 It should be emphasized that redo PTA or stenting itself carries a risk of damaging the stent’s stability. In addition, one study showed that overlapping carotid stents predispose to thrombosis.1
A combination of methods such as mechanical thrombectomy with thrombus aspiration may be used according to ASA/AHA guidelines in patients with large segment occlusion who have not responded to intravenous thrombolysis and should be performed only by certified experts.31 According to literature data, mechanical thrombectomy and stenting may be associated with higher recanalization rates and improved functional status when compared to intra-arterial thrombolysis12.
In the most comprehensive review up to date in which 26 cases of early carotid stent thrombosis were presented an algorithm for the management has been proposed.1 This algorithm distinguishes whether the complication occurred intra- or post-procedurally. In the latter case, an imaging study initially such as carotid duplex examination, followed by digital substraction angiography or computed tomographic angiography in suspicion of distal extension of carotid thrombosis is recommended to evaluate the level of thrombosis. Once confirmed, then percutaneous mechanical thrombectomy, thromboaspiration and thrombolysis or thrombolysis with or without IIb/IIIa receptor inhibitors are suggested. Then, if partial or residual intrastent thrombosis with no distal cerebral extension is documented surgical exploration can be used. If carotid stent thrombosis occurs intraprocedurally immediate treatment with percutaneous mechanical thrombectomy, thromboaspiration and thrombolysis or thrombolysis with or without IIb/IIIa receptor inhibitors should be initiated. If the thrombus is refractory, surgical exploration should be considered. Tirofiban has been suggested mainly due to its short platelet-bound half-life and long plasma half-life predisposing to lower hemorrhagic risk1.
In conclusion, acute carotid stent thrombosis is a rare complication of CAS with potentially devastating even lethal outcomes. Although, there is no consensus on its management, thrombolysis, mechanical thrombectomy, thromboaspiration with thrombolysis, open surgical treatment, and re angioplasty have all been used, depending on the stent thrombosis time and cause with promising results. The critical points in preventing a catastrophic outcome are immediate recognition of thrombosis and rapid revascularization of the damaged tissue.
References
- Moulakakis KG, Mylonas SN, Lazaris A, Tsivgoulis G, Kakisis J, Sfyroeras GS et al. Acute Carotid Stent Thrombosis: A Comprehensive Review. Vasc Endovascular Surg. 2016;50:511-521.
- Chaturvedi S, Sohrab S, Tselis A. Carotid stent thrombosis: report of 2 fatal cases. Stroke. 2001;32:2700-2.
- Kahyaoglu M, Velioglu M, Gecmen C, Kalayci A, Cakmak EO, Izgi İA. Acute carotid stent thrombosis. J Cardiovasc Thorac Res. 2018;10:243-245.
- Kwon OK, Kim SH, Jacobsen EA, Marks MP. Clinical implications of internal carotid artery flow impairment caused by filter occlusion during carotid artery stenting. AJNR Am J Neuroradiol. 2012;33:494-9.
- Adams HP Jr, Effron MB, Torner J, Dávalos A, Frayne J, Teal Pet al.; AbESTT-II Investigators. Emergency administration of abciximab for treatment of patients with acute ischemic stroke: results of an international phase III trial: Abciximab in Emergency Treatment of Stroke Trial (AbESTT-II). Stroke. 2008;39:87-99.
- Steiner-Böker S, Cejna M, Nasel C, Minar E, Kopp CW. Successful revascularization of acute carotid stent thrombosis by facilitated thrombolysis.
- AJNR Am J Neuroradiol. 2004;25:1411-3
- SRTEINER RL, Bhama JK, Lin PH, Lumsden AB. Transient ischemic attack due to early carotid stent thrombosis: successful rescue with rheolytic thrombectomy and systemic abciximab. J Endovasc Ther. 2003;10:870-4.
- Tong FC, Cloft HJ, Joseph GJ, Samuels OB, Dion JE. Abciximab rescue in acute carotid stent thrombosis. AJNR Am J Neuroradiol. 2000;21:1750-2.
- Hamann GF, Liebetrau M, Pfefferkorn T, Heiss MM. Successful systemic thrombolysis for carotid stent thrombosis. Eur Neurol. 2002;48:37-9.
- Paciaroni M, Balucani C, Agnelli G, Caso V, Silvestrelli G, Grotta JC, et al. Systemic thrombolysis in patients with acute ischemic stroke and Internal Carotid ARtery Occlusion: the ICARO study. Stroke. 2012;43:125-30.
- H A, Grosz C, Lazar A. Acute carotid stent thrombosis: review of the literature and long-term follow-up. Cardiovasc Revasc Med. 2010;11:110-3.
- Kappelhof M, Marquering HA, Berkhemer OA, Majoie CB. Intra-arterial treatment of patients with acute ischemic stroke and internal carotid artery occlusion: a literature review. J Neurointerv Surg. 2015;7:8-15.
- Markatis F, Petrosyan A, Abdulamit T, Bergeron P. Acute carotid stent thrombosis: a case of surgical revascularization and review of treatment options. Vascular. 2012;20:217-20.
- Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BMet al.; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870-947.
- Kanemaru K, Nishiyama Y, Yoshioka H, Satoh K, Hashimoto K, Hanihara M et al. In-stent thrombosis after carotid artery stenting despite sufficient antiplatelet therapy in a bladder cancer patient. J Stroke Cerebrovasc Dis. 2013;22:1196-200.
- Munich S, Moftakhar R, Lopes D. Recanalization of acute carotid stent occlusion using Penumbra 4Max aspiration catheter: technical report and mreview of rescue strategies for acute carotid stent occlusion. BMJ Case Rep. 2013 14;2013: bcr2013010706.
- Dhall A, Malani SK, Chadha DS. Thrombosuction for procedural acute thrombosis during high-risk carotid angioplasty–a case report. J Invasive Cardiol. 2010 Aug;22(8):E144-6. PMID: 20679679.
- Owens EL, Kumins NH, Bergan JJ, Sparks SR. Surgical management of acute complications and critical restenosis following carotid artery stenting. Ann Vasc Surg. 2002 Mar;16(2):168-75. doi: 10.1007/s10016-001-0152-2. PMID: 11972247.
- Masuo O, Terada T, Matsuda Y, Ogura M, Tsumoto T, Yamaga H, Itakura T. Successful recanalization by in-stent percutaneous transluminal angioplasty with distal protection for acute carotid stent thrombosis. Neurol Med Chir (Tokyo). 2006;46:495-9.
- Hu W, Wang L, Wang G. Acute In-Stent Thrombosis after Carotid Angioplasty and Stenting: A Case Report and Literature Review. Interv Neurol. 2018;7:265-270.
- Setacci C, de Donato G, Setacci F, Chisci E, Cappelli A, Pieraccini M et al. A. Surgical management of acute carotid thrombosis after carotid stenting: a report of three cases. J Vasc Surg. 2005;42:993-6.
- Buhk JH, Wellmer A, Knauth M. Late in-stent thrombosis following carotid angioplasty and stenting. Neurology. 2006;66:1594-6.
- Choi HJ, Kim ST, Jeong YG, Jeong HW. Superficial temporal artery-middle cerebral artery anastomosis for internal carotid artery occlusion by subacute in-stent thrombosis after carotid artery stenting. J Korean Neurosurg Soc. 2012;52:551-4.
- Kim YW, Kang DH, Hwang JH, Park J, Hwang YH, Kim YS. Rescue strategy for acute carotid stent thrombosis during carotid stenting with distal filter protection using forced arterial suction thrombectomy with a reperfusion catheter of the Penumbra System: a technical note. Acta Neurochir (Wien). 2013;155:1583-8.
- Seo KD, Lee KO, Kim DJ, Lee KY. Rescue use of tirofiban for acute carotid in-stent thrombosis. Yonsei Med J. 2008;49:163-6.
- Köklü E, Arslan Ş, Yüksel İÖ, Bayar N, Koç P. Acute Carotid Artery Stent Thrombosis Due to Dual Antiplatelet Resistance. Cardiovasc Intervent Radiol. 2015;38:1011-4.
- Moulakakis KG, Kakisis J, Tsivgoulis G, Zymvragoudakis V, Spiliopoulos S, Lazaris A et al. Acute Early Carotid Stent Thrombosis: A Case Series. Ann Vasc Surg. 2017;45: 69-78.
- Wei W, Wang Y, Wang P, Li Z. Revascularization of acute stent thrombosis after carotid artery stenting in a CYP2C19*2 heterozygote patient. J Int Med Res. 2021;49:3000605211001191.
- Cvjetko I, Đaković Bacalja I, Cvjetko T. Acute Carotid Artery Stent Thrombosis. Cardiovasc Intervent Radiol. 2018;41:355-356
- Toljan K, Jovanović I, Starčević K, Ljevak J, Blažević N, Radoš M, Poljaković Z. Acute Carotid Stent Thrombosis in an Ultrarapid Clopidogrel Metabolizer: Case Report and Literature Review. Vasc Endovascular Surg. 2019;53:602-605.
- Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. American Heart Association Stroke Council. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49:e46-e110.